by Dr Isabeau Tindall, Curtin University, and Professor Warren Mansell, Curtin University
Transdiagnostic mental health interventions cover a vast array of different approaches. Here, we have provided an overview, with up-to-date links on their evidence base.
The field of transdiagnostic interventions is ever evolving, and so, this list is not exhaustive. In this blog, we have not considered the range of transdiagnostic child, adolescent, school and family interventions, nor the wide range of stress management and wellbeing interventions that also draw upon common principles that are not specific to any mental health diagnosis. Instead, we have focused on adult interventions for clinical symptoms, and we have separated this overview into two sections: limited range and wide range.
Limited Range
Transdiagnostic interventions that focus on commonalities across a limited range of diagnostic categories have been created for the treatment of eating disorders, psychosis, and anxiety disorders and unipolar depression.

Cognitive behaviour therapy for eating disorders
Eating disorders (e.g., anorexia nervosa and bulimia nervosa) share core features, such as the preoccupation with eating and body shape. One established intervention, based on a transdiagnostic theory for eating disorders (see Fairburn et al., 2003) that focuses on the treatment of these commonalities is cognitive behaviour therapy for eating disorders (CBT-ED; see Fairburn et al., 2009).
For more information on the empirical base supporting CBT-ED, see:
- Atwood and Friedman (2019) for a review
Adapted cognitive behaviour therapy
An intervention with emerging evidence for use with psychosis, specifically schizophrenia, non-affective psychotic disorder, and worry is adapted cognitive behaviour therapy (see Tarrier & Wykes, 2004). This intervention focuses on similarities between diagnoses, such as the atypical interpretation of experiences causing distress, rather than on treatment for a specific diagnosis.
For a review outlining the benefits of a transdiagnostic approach to psychosis, see:

Unified protocol

Transdiagnostic interventions for anxiety disorders and unipolar depression, centre on the shared features across diagnoses, such as negative affectivity (dispositional tendency to respond negatively to stimuli) and intolerance of uncertainty (belief that uncertain situations are dangerous). A well-established intervention targeting negative affect is the unified protocol (see Barlow et al., 2017) which aims to modify underlying negative emotions through psychoeducation, self-monitoring, and cognitive restructuring.
See below for links to a range of further transdiagnostic interventions effective for treatment within anxiety and unipolar depression:
- Norton (2012) for transdiagnostic CBT
- Dugas et al. (2003) for intolerance of uncertainty therapy
- Riccardi et al. (2017) for false safety behaviour elimination therapy
- Neacsiu et al. (2014) for dialectical behaviour therapy skills training
Meta-cognitive therapy
Based on the self-regulatory executive functioning model (see Wells & Matthews, 1996), meta-cognitive therapy has an evidence base for treatment within generalised anxiety disorder. Yet it has also been applied as a transdiagnostic intervention through addressing the metacognitive beliefs maintaining psychological distress.
For more information on meta-cognitive therapy, see:
- McEvoy (2019) for a review of its use with anxiety disorders
Wide Range
The transdiagnostic interventions below have been applied broadly across a wide range of diagnostic categories. Many of them have the potential to be applied for universal mental health and wellbeing. This is an advantage over the interventions covered above, where treatment was exclusive to a limited number of diagnostic categories.
Transdiagnostic sleep and circadian intervention
Sleep and circadian dysfunction such as insomnia and hypersomnia are symptoms of many mental disorders such as depression, psychosis, and anxiety.
The transdiagnostic sleep and circadian intervention (see Harvey, 2008) is a validated treatment for sleep and circadian dysfunction that consists of four cross-cutting modules (e.g., goal setting, circadian education), five core modules (e.g., irregular sleep-wake schedule, difficulty winding down) and four optional modules (e.g., poor sleep efficiencies).
For a randomised control trial supporting the use of the transdiagnostic sleep and circadian intervention, see:

CBT for low self-esteem
Low self-esteem occurs across mental health conditions, such as, anxiety, psychosis, and depression. Based on the cognitive model of low self-esteem (see Fennell, 2006), the CBT for low self-esteem (CBT-SE; see Fennell, 2007) protocol focuses on modifying the negative self-beliefs that maintain low self-esteem.
For a review of evidence specific to transdiagnostic approaches for self-esteem, please see:
CBT for perfectionism

Perfectionism (negative self-evaluation and the pursuit of high standards) is a common feature of numerous psychiatric disorders, such as eating disorders, obsessive compulsive disorder, and anxiety disorders. Underpinned by the cognitive model for perfectionism (see Egan et al., 2001), CBT for perfectionism (see Fairburn et al., 2003), is an intervention that has received promising preliminary evaluation. This approach focuses on identifying cognitive and behavioural components underlying perfectionism and uses cognitive behavioural techniques during treatment.
For a recent overview of evidence for CBT for perfectionism see:
Mindfulness
Mindfulness is a focus of many transdiagnostic interventions, including those that are limited range, such as mindfulness-based cognitive therapy for depression (see Segal et al., 2002), and mindfulness-based relapse prevention for alcohol and substance use disorders (see Witkiewitz et al., 2005), and those that are wide ranging, such as mindfulness-based stress reduction (see Baer, 2003).
For a review of evidence using mindfulness for psychological distress, see:

Compassion-focused therapy
Used in treatment for anxiety disorders, depression, anger, and eating disorders, compassion-focused therapy (Gilbert, 2009) focuses on developing compassionate skills to improve emotional regulation. This is based around the compassionate focused approach (see Gilbert, 2005), which indicates that experiencing high levels of threat and drive reduces the ability to self-sooth and regulate distress.
For a review of the effectiveness of compassion-focused therapy, see:
Paul Gilbert (copyright: JonRhodes – Own work, CC BY-SA 3.0)
Acceptance and commitment therapy
Acceptance and commitment therapy (ACT; Hayes et al., 1999), uses relational frame theory as a foundation (Hayes et al. 2001). ACT is widely supported for use with anxiety disorders, depression, substance use, and physical health conditions, among others. ACT uses specific methods such as mindfulness and behavior change techniques (e.g., goal setting) to reduce psychological distress.
For more details into the specifics of ACT, see:
- Gloster et al. (2020) for a recent review of evidence supporting ACT
Emotional-focused therapy
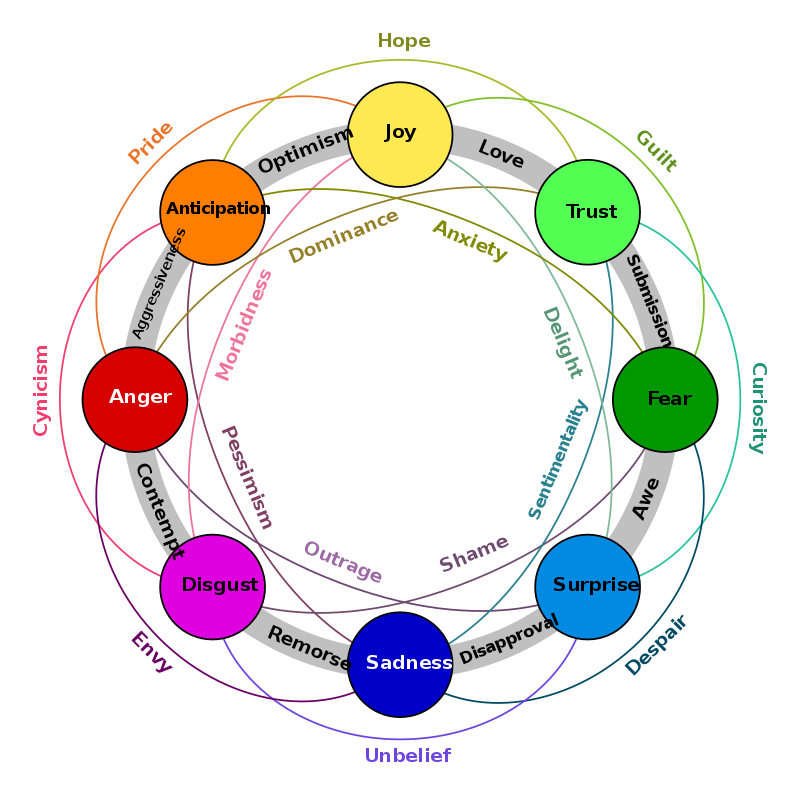
Emotion-focused therapy (EFT; Greenberg, 2004) is an intervention which focuses on enhancing and facilitating a clients ability to process their emotions. EFT has support for use within a wide range of settings (with couples, families, and individuals) and across an array of disorders, such as, anxiety, complex trauma, personality disorders, depression and eating disorders.
For more details into the use of EFT across a diverse range of settings, see:
- Osoro et al. (2021) for a review of evidence supporting the use of EFT within the treatment of eating disorders
- Ladislav et al. (2022) for a feasibility randomised control trial testing the suitability of EFT for generalised anxiety disorder
- Watson & Sharbenee, 2021 for a comprehensive overview of emotion-focused therapy
Copyright: ChaoticBrain – Own work, CC BY-SA 4.0
Method of levels therapy and take control course
Based on perceptual control theory (PCT; Powers, 1973), method of levels therapy (MOL; Carey, 2008) and the take control course (TCC; Morris et al., 2016), are two interventions with a growing evidence base for use within diverse populations. MOL aims to facilitate reorganisation through elevating awareness to the source of goal conflicts. The TCC is a group-based intervention that focuses primarily on psychoeducation. It is structured around discussion and exercises that facilitate the application of the principles of PCT.
For evidence regarding these interventions, see:
Method of levels
- Jenkins et al (2020) for a feasibility study of MOL within inpatient settings
- Griffiths et al. (2019) for a feasibility trial on MOL in psychosis
Take control course
- Morris et al. (2022) for a randomised non-inferiority trial of TCC within depression and anxiety
Psychodynamic psychotherapy
Psychodynamic psychotherapy refers to a number of related interventions that have their origins in psychodynamic theory (e.g. Malan, 1976; Berzoff et al., 2011), and have been applied to self-harm, depression, social anxiety disorder, and interpersonal problems.
To learn more about psychodynamic psychotherapy, see:
- Fonagy (2015) for a review of the effectiveness of psychodynamic psychotherapy across disorders

This Post Has 0 Comments